Earlier this year, researchers from the ETH Zurich team created a highly effective “gene switch” to deliver targeted cell therapy to people with diabetes. Diabetes has been a long-time health concern in the US, grouped into a category of diseases known as “metabolic diseases” and affecting one in every ten individuals. Although human bodies are designed to regulate blood sugar, this fails when the individual is affected by diabetes. However, cell therapy through the “gene switch” may be the answer to this.
A switch powered by nitroglycerine
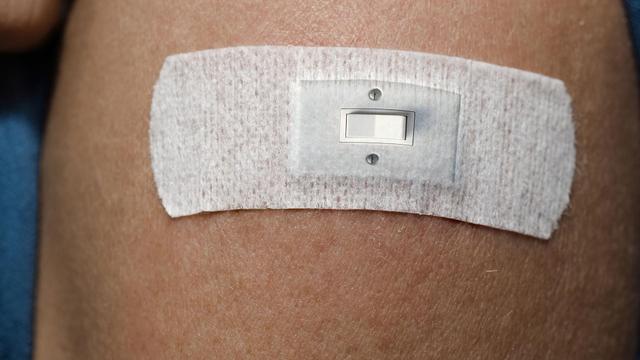
When the body attempts to limit blood sugar, it uses pancreatic cells, which are specialized cells that can regulate sudden spikes in blood sugar levels, such as after eating a meal. However, the system breaks down when someone has diabetes. Until now, individuals have been using insulin injections to control blood sugar levels, but this process is not as directed and accurate as the body’s methods. Scientists at ETH have begun to experiment with human cells, adding new genetic networks to them and giving them special functions that help fight diabetes. The idea would be that these cells are then injected into the skin, and would be able to be controlled by a switch. After multiple years of experimentation, scientists are using nitroglycerine, the ingredient found in chest pain relief products, to facilitate their innovation. “For me, this solution is the best gene switch that my group and I have built so far,” said Professor of Biotechnology and Bioengineering Martin Fussenegger at the Department of Biosystems Science and Engineering of ETH Zurich in Basel.
Cell therapy procedure
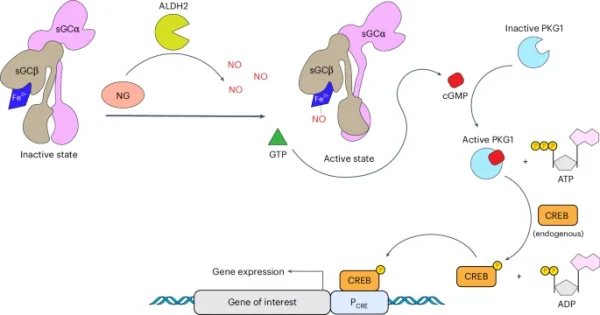
After time, the nitroglycerine will spread throughout the skin, and will eventually meet the engineered kidney cells. This process will turn the nitroglycerine into nitric acid, which will release a chemical called GLP-1. GLP-1 is a chemical which will tell the pancreas to release insulin, which will help regulate blood sugar levels in the body. GLP-1 will also help reduce appetite, which is good in the case of diabetes. Risk of immune system weakening is also not a possibility, as the switch is composed of only components involving materials that are found in the human body.
“That’s a new and groundbreaking feature. With components from other species, there is always a risk of false triggering, interference with the body’s own processes, or immune reactions. Here, we’re able to rule that out.” Martin Fussenegger, Professor of Biotechnology and Bioengineering, Department of Biosystems Science and Engineering, ETH Zurich.
The future of genetic switches
Currently, Fussenegger is putting his focus on diabetes, as it is the most widespread metabolic disease in the world. “That’s the model disease we work with. Fundamentally, however, it’s also possible to develop cell therapies for other metabolic, autoimmune or even neurodegenerative diseases – in principle, for everything that requires dynamic regulation.” Cell therapy holds a future that has the potential to cure all or many of the metabolic diseases in the world, such as Gaucher’s disease and Mitochondrial disease. Through extensive study by the ETH and other organizations, the end to metabolic diseases may come within reach.
RELATED STORIES:
https://interestingengineering.com/health/gene-switch-for-diabetes-cell-therapy
https://www.sciencedaily.com/releases/2025/02/250214123742.htm
https://news.google.com/search?q=diabetes&safe=active&surl=1&hl=en-US&gl=US&ceid=US:en
TAKE ACTION:
Donate to the American Diabetes Foundation to help people with diabetes. This money will help further research on diabetes, and help Americans who are fighting diabetes.
https://diabetes.org/ways-to-give
If you are a professional, apply for a job at ETH Zurich to further research in this field.